Sleep apnea is a serious sleep disorder that can have significant health implications. As this condition becomes increasingly recognized, many people are seeking information about testing and treatment options. Medicare, the federal health insurance program for seniors and certain disabled individuals, offers specific coverage related to sleep apnea tests. In this article, we will explore whether Medicare covers sleep apnea tests, the options available, and how to navigate this important aspect of healthcare.
Understanding Medicare Coverage
Before diving into specific coverage for sleep apnea tests and how much is a sleep study costs, it’s essential to grasp the basics of how Medicare works. Medicare is divided into several parts, each serving different needs and health services.
Basics of Medicare
Medicare consists of four main parts: Part A, Part B, Part C, and Part D. Part A covers hospital insurance, including inpatient stays, skilled nursing facility care, hospice, and some home health care. Part B provides medical insurance, which covers outpatient care, doctor visits, preventive services, and some tests.
Part C, or Medicare Advantage, combines coverage from Parts A and B, often including additional benefits such as vision or dental coverage. Finally, Part D offers prescription drug coverage. Understanding these parts can help you navigate your options better. Each part has its own eligibility requirements and costs, which can vary significantly based on income and the specific plan chosen. For example, while Part A is usually premium-free for most beneficiaries, Part B requires a monthly premium, and the costs can increase based on income levels. This layered structure allows for a more tailored approach to healthcare, ensuring that beneficiaries can select the coverage that best fits their individual health needs. Click here to know when should you get sleep disorders tests.
Medicare and Sleep Apnea: A General Overview
Sleep apnea may qualify for coverage under Medicare, particularly if it is diagnosed as part of a sleep study conducted by a health care provider. Medicare recognizes the seriousness of sleep apnea and the necessity of appropriate testing and treatment to improve health outcomes and enhance the quality of life for affected individuals. The coverage typically includes both the diagnostic tests, such as polysomnography, and the necessary equipment, like CPAP machines, which are essential for managing the condition effectively.
By understanding the general overview of Medicare in conjunction with sleep apnea, patients can better advocate for their health and ensure they receive the medical attention they require. It’s important to note that Medicare may also cover follow-up consultations and ongoing therapy, which are critical for monitoring the effectiveness of treatment plans. Additionally, beneficiaries should be aware of the specific criteria that must be met for coverage, including documentation of symptoms and a formal diagnosis from a qualified healthcare provider. This proactive approach not only empowers patients but also facilitates a more comprehensive understanding of their healthcare journey, allowing them to make informed decisions about their treatment options and overall well-being.
Sleep Apnea Tests and Diagnosis
The diagnosis of sleep apnea typically involves specific testing mechanisms that can vary in complexity. Understanding these tests is crucial for recognizing what Medicare may cover.
What is Sleep Apnea?
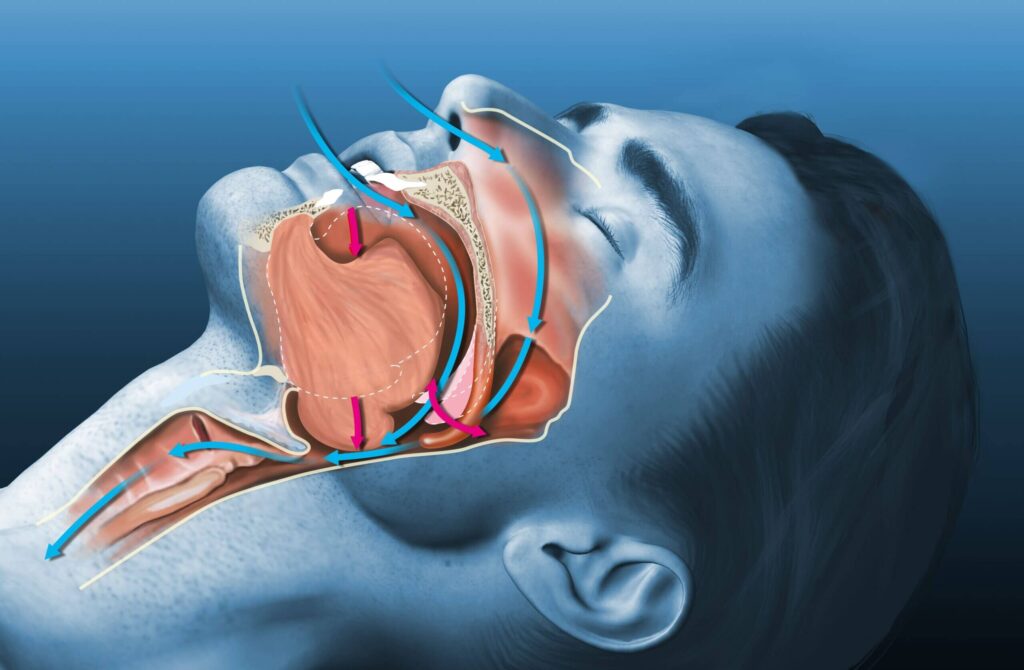
Sleep apnea is characterized by repeated interruptions in breathing during sleep, leading to reduced oxygen levels and frequent awakenings. People with sleep apnea may experience loud snoring and excessive daytime sleepiness, among other symptoms. This condition can lead to serious health issues, including heart disease, diabetes, and even stroke if left untreated. The impact of sleep apnea extends beyond physical health; it can also affect mental well-being, leading to issues such as anxiety and depression due to chronic fatigue and disrupted sleep patterns.
As more information emerges about the ramifications of sleep apnea, it is vital to seek diagnosis and treatment options that may be covered under Medicare. Early detection can significantly improve quality of life, as well as reduce the risk of developing more severe health complications. Patients are encouraged to discuss their symptoms openly with healthcare providers to facilitate timely intervention.
Types of Sleep Apnea Tests
There are several types of tests used to diagnose sleep apnea. These include:
- Polysomnography: A comprehensive sleep study conducted in a sleep lab that records brain waves, oxygen levels, heart rate, and breathing. This test often involves spending the night in a specialized facility where various sensors monitor your body’s activity during sleep.
- Home Sleep Apnea Testing: A simplified test performed in the comfort of your home, typically used for individuals with a high likelihood of having sleep apnea. This method is convenient and allows patients to undergo testing in a familiar environment, which can lead to more natural sleep patterns.
- Continuous Positive Airway Pressure (CPAP) Device Usage: While primarily used for treatment, CPAP devices can also track data that might aid in diagnosing sleep apnea. These devices monitor airflow and can provide valuable insights into the severity of the condition based on usage patterns and interruptions.
Understanding the different types of tests helps patients make informed decisions and ensures they are aware of what Medicare may cover. Additionally, it is important for patients to prepare for these tests by following any pre-test instructions provided by their healthcare provider, such as avoiding caffeine or alcohol, which can interfere with sleep quality. Being well-informed about the testing process can alleviate anxiety and lead to a more accurate diagnosis.
Medicare’s Coverage for Sleep Apnea Tests
Once a healthcare provider has determined that a sleep study is warranted, the next step is understanding what Medicare covers regarding these tests.
Criteria for Medicare Coverage
Medicare typically covers sleep apnea tests if a healthcare provider deems them medically necessary. Certain criteria must be met, including but not limited to:
- The patient must have symptoms of sleep apnea.
- A primary care physician must refer the patient for testing.
- The testing must be conducted in a Medicare-approved facility.
Understanding these criteria can help patients navigate the evaluation and testing process more efficiently. Additionally, it is beneficial for patients to keep a detailed record of their symptoms, such as excessive daytime sleepiness, loud snoring, and episodes of breathing cessation during sleep. This documentation can be invaluable during consultations with healthcare providers and may assist in justifying the need for testing to Medicare.
Coverage for Different Types of Sleep Apnea Tests
Medicare’s coverage of sleep apnea tests may vary based on the type of test performed. Generally, Medicare Part B covers both polysomnography and home sleep apnea testing, provided they meet the aforementioned criteria for medical necessity.
Polysomnography, often conducted in a sleep lab, involves comprehensive monitoring of various body functions during sleep, including brain activity, eye movement, heart rate, and oxygen levels. This detailed analysis can provide insights into the severity of sleep apnea and guide treatment options. On the other hand, home sleep apnea testing offers a more convenient alternative, allowing patients to undergo testing in the comfort of their own homes. However, it typically measures fewer parameters, which may limit the depth of information gathered. It’s important to consult with your healthcare provider about the specific type of testing recommended, as this will influence coverage and out-of-pocket costs. Furthermore, understanding the nuances of each testing method can empower patients to make informed decisions about their health care options and preferences.
Out-of-Pocket Costs for Sleep Apnea Tests
While Medicare provides coverage, beneficiaries may still encounter out-of-pocket expenses. Understanding these costs is crucial for financial planning and managing health care expenses.
Understanding Co-pays and Deductibles
Medicare generally requires beneficiaries to pay a deductible and a co-pay for each service they receive. For sleep apnea tests, the specifics can vary depending on your plan and the type of test performed. Beneficiaries should review their policy details and communicate with their healthcare provider to understand potential financial liabilities.
It’s also essential to keep an eye on changes in Medicare policies, as updates may impact co-pays and deductibles related to sleep apnea tests and subsequent treatments. Moreover, understanding how these costs fit into your overall healthcare budget can help you prepare for any unexpected expenses that may arise during your treatment journey.

Estimating Your Potential Costs
Estimating potential costs for sleep apnea tests can be done by reviewing your Medicare summary notice and connecting with your healthcare provider’s billing department. Patients should ask about the expected out-of-pocket costs, including co-pays and deductibles, to make informed financial decisions.
Additionally, some individuals may qualify for financial assistance or programs that can help mitigate these costs, so exploring options is prudent. It’s important to inquire about any available payment plans or sliding scale fees that may be offered by testing facilities, as these can significantly reduce the financial burden associated with sleep apnea testing. Furthermore, some non-profit organizations and advocacy groups may provide resources or guidance on navigating the complexities of healthcare costs, ensuring that patients are not left to manage these challenges alone.
Navigating Medicare’s Policies on Sleep Apnea
Understanding and navigating Medicare’s policies can be challenging but essential for those suffering from sleep apnea. It’s important to be well-informed to maximize your health benefits.
How to Apply for Coverage
To apply for Medicare coverage for sleep apnea tests, beneficiaries should first consult their primary care physician, who can provide referrals based on medical necessity. After receiving a recommendation, you can schedule testing at an approved facility. These tests may include a polysomnography, which is an overnight sleep study that monitors various body functions during sleep, or a home sleep apnea test, which is a more convenient option that can be done in the comfort of your own home.
Always keep documentation regarding referrals and communications with healthcare providers, as this information may be necessary when applying for coverage or submitting claims. Additionally, it’s wise to familiarize yourself with the specific criteria that Medicare uses to determine coverage eligibility, as this can vary by individual circumstances. Understanding the nuances of your policy can help you avoid unexpected out-of-pocket expenses.
Appealing a Medicare Decision
If a claim for a sleep apnea test is denied, beneficiaries have the right to appeal the decision. The appeal process generally involves:
- Reviewing the denial notice and understanding the reasons for denial.
- Gathering any additional supporting documentation.
- Filing an appeal through the appropriate Medicare channels.
Appealing a decision can be a complex process, so it’s beneficial to consult with a Medicare advocate or a healthcare professional who can assist you in navigating the appeal successfully. It’s also helpful to connect with support groups or online forums where others share their experiences with Medicare appeals, as these communities can provide valuable insights and encouragement. Remember that persistence is key; many beneficiaries find success in their appeals after thorough preparation and follow-up.
Moreover, it’s essential to stay informed about any changes in Medicare policies regarding sleep apnea, as regulations can evolve. Regularly checking the official Medicare website or subscribing to updates can ensure you have the latest information at your fingertips. This proactive approach can empower you to make informed decisions about your health care and ensure that you receive the necessary support for managing your sleep apnea effectively.